Dental insurance coordination of benefits Idea
Home » Trend » Dental insurance coordination of benefits IdeaYour Dental insurance coordination of benefits images are available. Dental insurance coordination of benefits are a topic that is being searched for and liked by netizens now. You can Get the Dental insurance coordination of benefits files here. Find and Download all royalty-free vectors.
If you’re searching for dental insurance coordination of benefits pictures information linked to the dental insurance coordination of benefits interest, you have come to the ideal site. Our site frequently provides you with suggestions for viewing the highest quality video and picture content, please kindly surf and locate more informative video articles and images that fit your interests.
Dental Insurance Coordination Of Benefits. There are 3 main scenarios where coordination of benefits comes into effect. Cda practice support receives hundreds of calls each year concerning the coordination of benefits when a patient has more than one dental plan for coverage. Coordination of benefits takes place when a patient has coverage under more than one dental insurance plans and both the plans have cob provisions. Best answer is yes, but read the plans very carefully.they can be tricky.
 Understanding Dual Coverage Dental Insurance From forestwooddentistry.ca
Understanding Dual Coverage Dental Insurance From forestwooddentistry.ca
The claim first goes to the insurer, if the primary plan does not cover the full amount of the treatment, then it is paid by the secondary plan. Coordination of benefits (cob) is the process of determining which of two or more insurance policies will have the primary responsibility of processing/paying a claim and the extent to which the other policies will contribute. However, it is important to note that there would never be doubling of benefits but a calculated sharing of the coverage costs between both the insurance carriers involved. “dual coverage” refers to when a patient’s dental treatment is covered by more than one dental benefits plan. Best answer is yes, but read the plans very carefully.they can be tricky. In order for delta dental of kansas to coordinate benefits with another insurance company, the patient must complete our dual coverage information request form located here so that we.
This comes into play when a patient filing a claim is covered under more than one dental plan.
What is coordination of benefits in dental insurance? There are 3 main scenarios where coordination of benefits comes into effect. Standard cob allows secondary dental plans to pay up to 100% of the covered service, i.e., the primary plan pays the service at 80%, and the secondary could pick up the remaining 20%. Every july, cda practice support starts hearing from members who have received notice from a dental benefit plan about a forthcoming audit. Coordination of benefits takes place when a patient is entitled to benefits from more than one dental plan. What is coordination of benefits in dental insurance coverage?
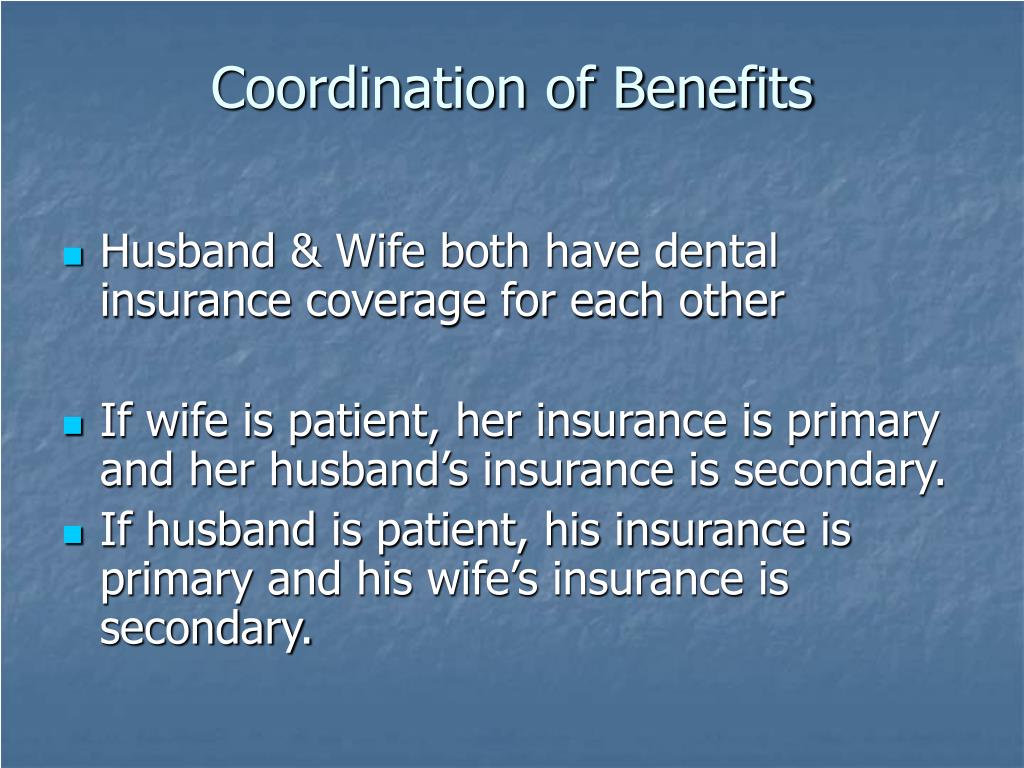 Source: slideserve.com
Source: slideserve.com
Both insurance companies are going to have to work together in order to make. This is when the secondary plan payment is based on the balance left after the primary has paid, but does not exceed the amount it would have paid as primary or the total amount of the claim. What does coordination of benefits mean in dental this term refers to how each policy is going to pay when a claim is generated. Also, ask your dentist how much the total charges will be. Every july, cda practice support starts hearing from members who have received notice from a dental benefit plan about a forthcoming audit.
 Source: caplinedentalservices.com
Source: caplinedentalservices.com
There are 3 main scenarios where coordination of benefits comes into effect. This comes into play when a patient filing a claim is covered under more than one dental plan. Understanding coordination of benefits and dual coverage page 1 of 2 sample of coordination of benefits procedure primary carrier pays 80% secondary carrier pays 20% patient pays cleaning $95 $76 $19 $0 you may be covered by two dental plans if you have two jobs that both provide dental benefits or if you are covered by your spouse’s What is coordination of benefits in dental insurance coverage? The plans will coordinate the benefits to eliminate over insurance or duplication of benefits.
 Source: caplinedentalservices.com
Source: caplinedentalservices.com
Below are the types of cob that determine how patient coverage gets settled to avoid dental claim denial. Nov 28, 2016 — coordination of benefits can often reduce your costs. What is coordination of benefits in dental insurance? This term refers to how each policy is going to pay when a claim is generated. The claim first goes to the insurer, if the primary plan does not cover the full amount of the treatment, then it is paid by the secondary plan.
 Source: pinterest.com
Source: pinterest.com
The claim first goes to the insurer, if the primary plan does not cover the full amount of the treatment, then it is paid by the secondary plan. Ada guidance on coordination of benefits. If you have more than one insurance plan, your insurers can “coordinate” if you file a (17). Best answer is yes, but read the plans very carefully.they can be tricky. Coordination of benefits takes place when a patient is entitled to benefits from more than one dental plan.
 Source: avitusdental.com
Source: avitusdental.com
Coordination of benefits (cob) is the process of determining which of two or more insurance policies will have the primary responsibility of processing/paying a claim and the extent to which the other policies will contribute. Also, ask your dentist how much the total charges will be. It is a term that describes when an individual is covered by more than one dental insurance policy. For example, bob and sarah johnson both have dental coverage. Coordination of benefits is a term that is frequently used in the area of dental insurance.
 Source: newsstellar.com
Source: newsstellar.com
Best answer is yes, but read the plans very carefully.they can be tricky. But knowing and understanding these rules can help dental practices avoid insurance denials and collect more. Coordination of benefits between the insurances helps to bring down the overall insurance costs for the patients. Coordination of benefits is a term that is frequently used in the area of dental insurance. Coordination of benefits takes place when a patient is entitled to benefits from more than one dental plan.
 Source: youtube.com
Source: youtube.com
This term refers to how each policy is going to pay when a claim is generated. Coordination of benefits between the insurances helps to bring down the overall insurance costs for the patients. Typically, the plan in which you are the main policyholder is your primary. What is coordination of benefits in dental insurance coverage? Below are the types of cob that determine how patient coverage gets settled to avoid dental claim denial.
 Source: forestwooddentistry.ca
Source: forestwooddentistry.ca
Ddks uses standard coordination of benefits. Dental teams often struggle with keeping the rules of coordination of benefits straight. Patients with more than one dental benefits program from state licensed carriers are likely to visit their dentists more frequently, knowing all or at least a large majority of treatment costs will be covered by the combination of two programs. Coordination of benefits takes place when a patient is entitled to benefits from more than one dental plan. This term refers to how each policy is going to pay when a claim is generated.
 Source: lcfowpa.com
Source: lcfowpa.com
Also, ask your dentist how much the total charges will be. Coordination of benefits is a term that is frequently used in the area of dental insurance. It also means the order in which the dental practice is held accountable for filing insurance claims. Understanding coordination of benefits and dual coverage page 1 of 2 sample of coordination of benefits procedure primary carrier pays 80% secondary carrier pays 20% patient pays cleaning $95 $76 $19 $0 you may be covered by two dental plans if you have two jobs that both provide dental benefits or if you are covered by your spouse’s In order for delta dental of kansas to coordinate benefits with another insurance company, the patient must complete our dual coverage information request form located here so that we.
 Source: caplinedentalservices.com
Source: caplinedentalservices.com
Dental it’s something we are familiar with in dentistry, coordination of benefits between carriers. In order for delta dental of kansas to coordinate benefits with another insurance company, the patient must complete our dual coverage information request form located here so that we. General coordination of benefits rules “coordination of benefits” is the process insurance companies follow to ensure that the combined benefits from all group dental plans do not exceed 100 percent of the dentist’s fee. What is coordination of benefits in dental insurance?
 Source: clipartkey.com
Source: clipartkey.com
The claim first goes to the insurer, if the primary plan does not cover the full amount of the treatment, then it is paid by the secondary plan. Coordination of benefits takes place when a patient has coverage under more than one dental insurance plans and both the plans have cob provisions. Every july, cda practice support starts hearing from members who have received notice from a dental benefit plan about a forthcoming audit. What is coordination of benefits in dental insurance coverage? Often times when you have a primary and a secondary dental carrier the secondary will not duplicate benefits paid by the primary.
 Source: learn.dentalclaimsacademy.com
Source: learn.dentalclaimsacademy.com
The claim first goes to the insurer, if the primary plan does not cover the full amount of the treatment, then it is paid by the secondary plan. The american dental association weighs in on defining the types of cob that affect payment of claims. Dental it’s something we are familiar with in dentistry, coordination of benefits between carriers. Coordination of benefits takes place when a patient has coverage under more than one dental insurance plans and both the plans have cob provisions. Cda practice support receives hundreds of calls each year concerning the coordination of benefits when a patient has more than one dental plan for coverage.
.jpg “4 coordination of benefits rules every dental practice”) Source: newsstellar.com
If you have more than one insurance plan, your insurers can “coordinate” if you file a (17). Dental teams often struggle with keeping the rules of coordination of benefits straight. What is coordination of benefits in dental insurance? Standard cob allows secondary dental plans to pay up to 100% of the covered service, i.e., the primary plan pays the service at 80%, and the secondary could pick up the remaining 20%. Coordination of benefits establishes the order claims are paid, known as primary, secondary, tertiary, quaternary, etc.
 Source: tennessee.deltadental.com
Coordination of benefits is a term that is frequently used in the area of dental insurance. Often times when you have a primary and a secondary dental carrier the secondary will not duplicate benefits paid by the primary. “dual coverage” refers to when a patient’s dental treatment is covered by more than one dental benefits plan. Cda practice support receives hundreds of calls each year concerning the coordination of benefits when a patient has more than one dental plan for coverage. General coordination of benefits rules
 Source: pinterest.com
Source: pinterest.com
Typically, the plan in which you are the main policyholder is your primary. Coordination of benefits (cob) is the procedure your insurance companies use to determine which one covers procedures first and which plan picks up as secondary. Typically, the plan in which you are the main policyholder is your primary. Coordination of benefits establishes the order claims are paid, known as primary, secondary, tertiary, quaternary, etc. Below are the types of cob that determine how patient coverage gets settled to avoid dental claim denial.
 Source: tn.deltadental.com
Dental it’s something we are familiar with in dentistry, coordination of benefits between carriers. This is when the secondary plan payment is based on the balance left after the primary has paid, but does not exceed the amount it would have paid as primary or the total amount of the claim. Legally, coordination of benefits (cob) has a specific sequence. Coordination of benefits between the insurances helps to bring down the overall insurance costs for the patients. Dental teams often struggle with keeping the rules of coordination of benefits straight.
 Source: healthnetwork.com
Source: healthnetwork.com
Every july, cda practice support starts hearing from members who have received notice from a dental benefit plan about a forthcoming audit. There are 3 main scenarios where coordination of benefits comes into effect. Yes, a patient can have four plans in some instances! Learn 10 standard cob rules. “dual coverage” refers to when a patient’s dental treatment is covered by more than one dental benefits plan.
 Source: fluenceportland.com
Source: fluenceportland.com
But knowing and understanding these rules can help dental practices avoid insurance denials and collect more. Coordination of benefits (cob) is the process of determining which of two or more insurance policies will have the primary responsibility of processing/paying a claim and the extent to which the other policies will contribute. What does coordination of benefits mean in dental this term refers to how each policy is going to pay when a claim is generated. Typically, the plan in which you are the main policyholder is your primary. Legally, coordination of benefits (cob) has a specific sequence.
This site is an open community for users to share their favorite wallpapers on the internet, all images or pictures in this website are for personal wallpaper use only, it is stricly prohibited to use this wallpaper for commercial purposes, if you are the author and find this image is shared without your permission, please kindly raise a DMCA report to Us.
If you find this site beneficial, please support us by sharing this posts to your favorite social media accounts like Facebook, Instagram and so on or you can also bookmark this blog page with the title dental insurance coordination of benefits by using Ctrl + D for devices a laptop with a Windows operating system or Command + D for laptops with an Apple operating system. If you use a smartphone, you can also use the drawer menu of the browser you are using. Whether it’s a Windows, Mac, iOS or Android operating system, you will still be able to bookmark this website.

Category
Related By Category
- Craft insurance arab al Idea
- Colonial life insurance claims Idea
- Business insurance and benefits information
- Deans and homer insurance Idea
- Crown cost without insurance information
- Delmonico insurance syracuse ny Idea
- Department of insurance and financial services michigan duties information
- Cost of eye exam with insurance Idea
- Cashless hospital list under national insurance company Idea
- Crowel insurance agency information